Medicinal mushrooms have been a favorite of mine for several years, going back to when I was in Naturopathic school looking for something to help a concussion patient. At that time, I found some research about the benefits of lion’s mane for nerves and the regeneration of the myelin sheath. At that time, I was told nothing could repair the myelin sheath. The myelin sheath is a sheath that forms around particular nerves (eg. the spinal cord and brain matter (aka. white matter)). It allows for the faster transmission of nerve messages up and down the spine and to the brain. The fact that this unsuspecting mushroom could help recover the myelin sheath was and still is extremely exciting.
In recent years, medicinal mushrooms have gained significant attention for their various actions, including supporting the immune system. Known for their centuries-old use in traditional medicine, mushrooms such as reishi, shiitake, turkey tail, lion mane, and maitake offer a natural way to support and balance the immune system. Scientific research is increasingly validating the health benefits of these fungi, making them popular supplements in modern wellness routines.
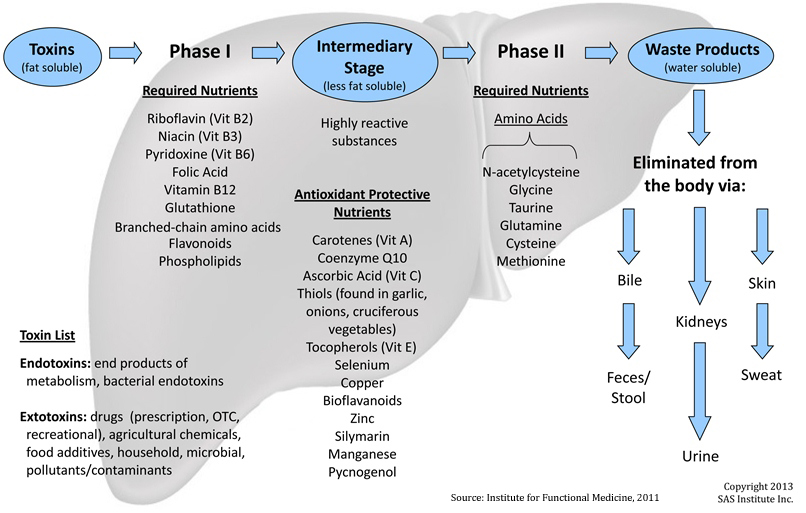
Our immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens. Maintaining a robust immune system is essential for preventing illness and promoting overall well-being. Medicinal mushrooms are rich in bioactive compounds like beta-glucans, polysaccharides, triterpenoids, and antioxidants, which are believed to modulate immune function, reduce inflammation, and improve the body's ability to ward off infections.
Reishi (Ganoderma lucidum)
Reishi, also known as the "mushroom of immortality," has been used in traditional Chinese medicine for over 2,000 years. Studies have shown that reishi contains powerful polysaccharides, triterpenoids, and peptidoglycans that can stimulate and support the immune system.
A study published by Wachtel-Galor S, et al, found that reishi enhances the activity of macrophages, natural killer (NK) cells, and other immune system components, contributing to improved defense mechanisms against infections and cancers. Reishi’s immune-modulating effects are valuable for reducing inflammation and regulating immune responses, which can benefit people with autoimmune disorders.
Turkey Tail (Trametes versicolor)
Turkey tail is another highly researched medicinal mushroom known for its immune-boosting properties. It contains polysaccharide-K (PSK) and polysaccharide-peptide (PSP), two compounds with powerful immune-enhancing effects.
An observational case study by, Stamets P, showed that turkey tail mushrooms helped improve immune recovery after radiotherapy with those with breast cancer. Different components of turkey tail have been seen to help improve the immune recovery of patients with breast, lung, and colon cancer, based on the National Cancer Institute.
Shiitake (Lentinula edodes)
Shiitake mushrooms are well-known for their culinary uses, but they also possess potent medicinal properties. They are particularly rich in lentinan, a type of beta-glucan, which is recognized for its ability to enhance immune function.
Research published in The Journal of the American College of Nutrition found that daily consumption of shiitake mushrooms increased sIgA production, and decreased inflammation as seen through CRP (C-Reactive Peptide). The study concluded that shiitake mushrooms have a dual role in supporting both innate and adaptive immune responses, making them a versatile option for immune health.
Maitake (Grifola frondosa)
Maitake, or "dancing mushroom," is another potent immune-boosting fungus. It contains a specific beta-glucan called D-fraction, which has been studied for its role in enhancing immune activity and fighting tumors.
A study by Xiaoshuang Dai, et al, showed that maitake D-fraction increased the proliferation, differentiation, and activation of immunocompetent cells - specifically the T-helper 1 dominant response. Additionally, maitake's ability to regulate immune responses makes it a useful supplement for people looking to maintain overall immune balance.
lion’s mane (Hericium erinaceus)
Lion’s mane is a culinary mushroom known for its affinity for the nervous system, and the ‘tubes of the body’ (eg. lymphatic system, nervous system, circulatory system, etc.). It contains several various compounds including polysaccharides, hericenone and erinacine, etc. These two compounds are from the fruiting body of lions mane and exhibit activity promoting Nerve Growth Factor (NGF) synthesis. Which allows it to regulate the stress response and regulating the health of neurons.
A study by Koichiro Mori, et al, showed that lion’s mane has anti-inflammatory effects on the macrophages that prevent fat tissue inflammation that is often associated with obesity. This makes lions mane a useful supplement for people who want to support their immune systems and nervous system.
The Science Behind Medicinal Mushrooms: How They Work
One of the key reasons medicinal mushrooms are so effective at supporting the immune system is their ability to act as immunomodulators. This means they help regulate the immune system, either stimulating it when it is underactive or calming it down when it is overactive. This makes mushrooms particularly valuable for individuals who need support with their immune system.
Medicinal mushrooms also contain beta-glucans, which are complex polysaccharides that can activate various immune cells, such as macrophages, dendritic cells, and NK cells . Beta-glucans work by binding to receptors on immune cells, triggering a cascade of immune responses that improve the body's ability to fight infections and abnormal cells.
Incorporating Medicinal Mushrooms into Your Diet
Medicinal mushrooms are available in various forms, including powders, capsules, extracts, and teas. I prefer a powdered form, to allow for easier dose adjustment, and adding it to my hot beverage or soup. When choosing a mushroom supplement, it’s important to look for products that are organic, non-GMO, and free from contaminants.
While medicinal mushrooms are generally safe for most people, those with certain medical conditions or those taking immunosuppressant drugs should consult a Naturopathic Doctor before incorporating mushrooms into their routine.
Medicinal mushrooms are powerful allies in supporting and maintaining a healthy immune system. Scientific research continues to validate their traditional use, particularly for their ability to moducate the immune function and help the body respond to infections and diseases. Whether you're looking to boost your immunity naturally or support overall wellness, mushrooms like reishi, turkey tail, shiitake, and maitake provide a safe and effective option backed by both tradition and science.
~Dr. Charmagne
References:
Wachtel-Galor S, Yuen J, Buswell JA, et al. Ganoderma lucidum (Lingzhi or Reishi): A Medicinal Mushroom. In: Benzie IFF, Wachtel-Galor S, editors. Herbal Medicine: Biomolecular and Clinical Aspects. 2nd edition. Boca Raton (FL): CRC Press/Taylor & Francis; 2011. Chapter 9.
Seweryn E, Ziała A, Gamian A. Health-Promoting of Polysaccharides Extracted from Ganoderma lucidum. Nutrients. 2021 Aug 7;13(8):2725. doi: 10.3390/nu13082725. PMID: 34444885; PMCID: PMC8400705.
Wang X, Lin Z. Immunomodulating Effect of Ganoderma (Lingzhi) and Possible Mechanism. Adv Exp Med Biol. 2019;1182:1-37. doi: 10.1007/978-981-32-9421-9_1. PMID: 31777013.
Jin X, Ruiz Beguerie J, Sze DM, et al.: Ganoderma lucidum (Reishi mushroom) for cancer treatment. Cochrane Database Syst Rev 6: CD007731, 2012.
Stamets P. Trametes versicolor (Turkey Tail Mushrooms) and the Treatment of Breast Cancer. Glob Adv Health Med. 2012 Nov;1(5):20. doi: 10.7453/gahmj.2012.1.5.007. Epub 2012 Nov 1. PMID: 27257526; PMCID: PMC4890100.
National Cancer Institute. Medicinal Mushrooms (PDQ(R)- Health Professional Version. https://www.cancer.gov/about-cancer/treatment/cam/hp/mushrooms-pdq#_7. Accessed: Sept 23, 2024
Cui J, Chisti Y. Polysaccharopeptides of Coriolus versicolor: physiological activity, uses, and production. Biotechnol Adv. 2003 Apr;21(2):109-22. doi: 10.1016/s0734-9750(03)00002-8. PMID: 14499133.
Dai, X., Stanilka, J. M., Rowe, C. A., & Percival, S. S. (2015). Consuming Lentinula edodes (shiitake) mushrooms daily improves human immunity: A randomized dietary intervention in healthy young adults. The Journal of the American College of Nutrition, 34(6), 478-487.
Harada, K., Saito, Y., & Satake, H. (2018). Maitake D-fraction and its synergistic anti-cancer effects. Annals of Translational Medicine, 6(2), 21
Bhoite R, Satyavrat V, Premasudha Sadananda M. Clinical benefits of β-glucan supplementation in children: a review. Discov Food. 2022;2(1):37. doi: 10.1007/s44187-022-00038-0. Epub 2022 Dec 27. PMCID: PMC9793387.
Mori K, Ouchi K, Hirasawa N. The Anti-Inflammatory Effects of Lion's Mane Culinary-Medicinal Mushroom, Hericium erinaceus (Higher Basidiomycetes) in a Coculture System of 3T3-L1 Adipocytes and RAW264 Macrophages. Int J Med Mushrooms. 2015;17(7):609-18. doi: 10.1615/intjmedmushrooms.v17.i7.10. PMID: 26559695.
Kostanda E, Musa S, Pereman I. Unveiling the Chemical Composition and Biofunctionality of Hericium spp. Fungi: A Comprehensive Overview. Int J Mol Sci. 2024 May 29;25(11):5949. doi: 10.3390/ijms25115949. PMID: 38892137; PMCID: PMC11172836.