Concussions are considered a type of Traumatic Brain Injury (TBI), and it is common in car accidents and sports. They occur when the head receives an external impact that causes the head and brain to shake rapidly (CDC, 2019). This can cause chemical changes within the brain, inflammation, bruising, and can cause damage to brain cells. While most people recover from concussions on their own, others have long-term consequences where they experience changes in mood, and cognition (eg. slower mental processing, worsening of memory, etc.). Those who experience multiple concussions may notice that it takes them longer and longer to recover, and others may find that some symptoms stay after months or years.
Some signs and symptoms that can be experienced with concussions are:
Amnesia of events before or after the head impact
Mood, behaviour, or personality changes
Being dazed or stunned
Uncoordinated movements (eg. balance problems)
Loss of consciousness
Headache or pressure in their head
Nausea or vomiting
Dizziness, blurry vision, or seeing double
Light or noise sensitivity
Confusion, difficulty concentrating
Memory problems
Difficulty with sleep (sleeping too much or too little, difficulty sleeping)
Fatigue (CDC, 2019, Mayfield Clinic, 2018)
These signs and symptoms may show up minutes after the injury or can take hours or days to occur. So it is important to observe the person who was injured and support them if needed. The number one recommendation for concussions is to rest for the first few days after the injury. This will be enough for the majority of people, with their symptoms resolving in the next few weeks. However, based on some studies, 5-22% of people with concussions will experience persistent cognitive problems after the first few weeks (Gustavo, et al; 2022). These symptoms can persist over a month, and they may continue to experience these symptoms for months or years. So what are they supposed to do?
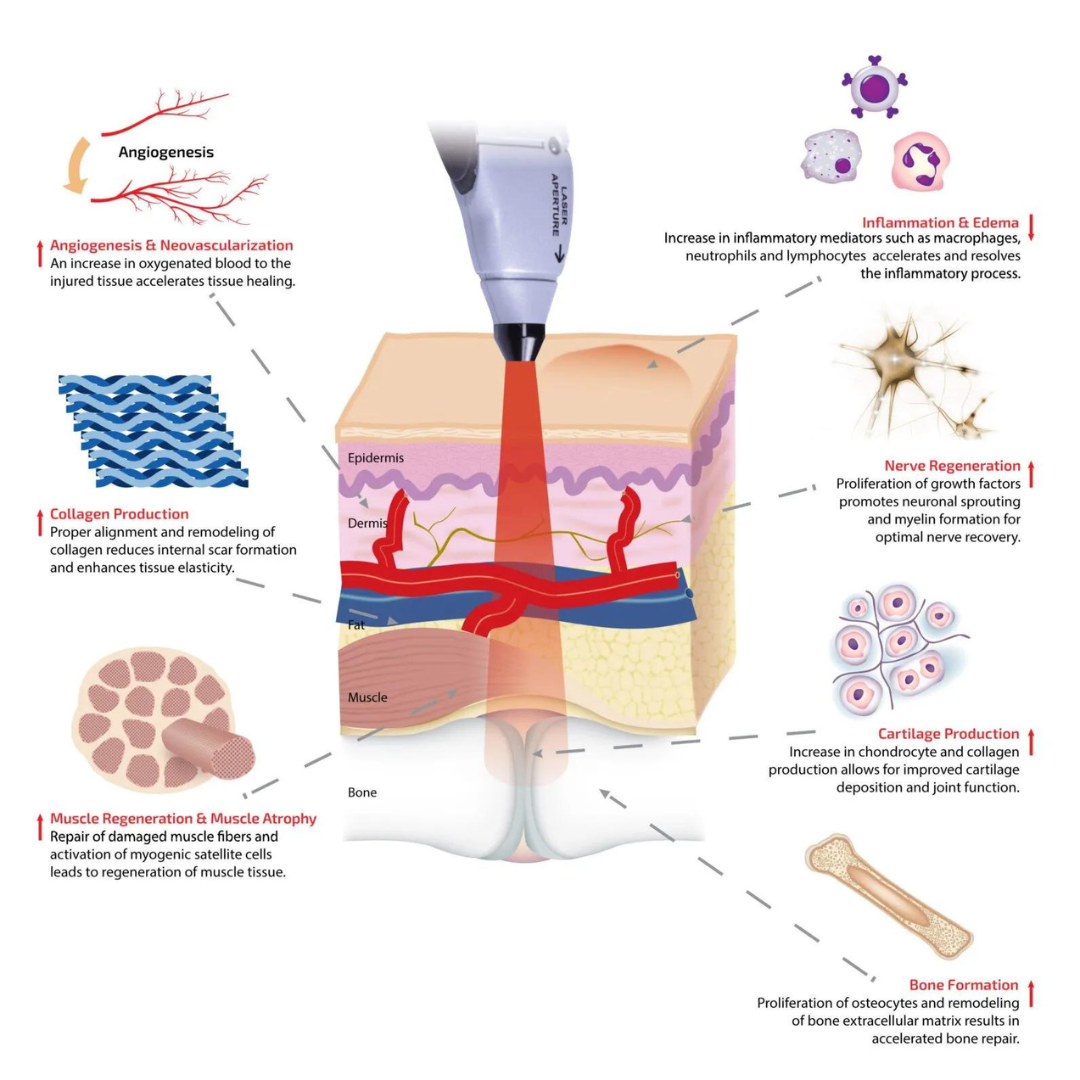
There aren’t currently any great treatments available for those experiencing post-traumatic symptoms. However, Photobiomodulation (also known as Low-Level Light Therapy, Cold Laser Therapy, or Laser Therapy) has been a tool of great interest since it is a non-invasive way to support those with post-traumatic symptoms. Photobiomodulation (PBM) is a wonderful therapy to use for TBI because it has many ways it helps support the healing of the brain. These include:
Increasing the ATP (the energy currency of the cell) production in the mitochondria through cytochrome C oxidase’s ability to absorb the photons from red light
Increasing regional brain flow by releasing the Nitric Oxide that tends to bind to the mitochondria and cause vasodilation
Anti-inflammatory and anti-oxidant effects by inhibiting the microglial activation (chronic activation causes neuronal degeneration)
Increases neurogenesis and synaptogenesis (new formation of neurons and improving their ability to communicate with each other) (Gustavo, et al; 2022) - this is particularly important for the recovery of the brain after TBI.
Studies have shown that PBM has been able to improve verbal memory, depression, executive function, headache, sleep disturbance, cognition, mood dysregulation, anxiety, irritability, work performance, blood flow to the brain, reduced swelling, inflammation, excitotoxicity, reduction in post-traumatic stress disorder in those with TBI (Naeser, et al; 2014, Gustavo, et al; 2022, Chao, et al; 2020). The amount and frequency of treatments varied between the studies, but it averaged 18 sessions over 7 weeks.
If this treatment interests you, you can click the link below to book an appointment.